Lipofilling in General
Introduction
Lipofilling (fat transfer or structural fat grafting) is now an established technique. It uses patients’ own fat as a permanent filler to add volume to soft tissues. The fat is harvested with thin cannulas, through small incisions, using conventional liposuction. After filtering, the isolated fat cells are then injected into the deficient area(s). In addition to adding volume, lipofilling reduces scarring, improving the quality and elasticity of the overlying skin. It’s mechanism of action is not fully understood but by repeated clinical application, this technique has demonstrated its safety and efficacy.
Lipofilling is used in soft tissue augmentation, body contouring, facial rejuvenation, facial reconstruction (e.g. Romberg’s disease) and breast surgery (both reconstructive and aesthetic).
Technique
Preoperatively, suitable donor site areas for fat harvesting are identified. These include the inner aspect of the knee, the thigh, the buttock, abdomen, love handles, back, upper inner arm and neck. The donor and recipient areas are photographed to compare pre- and postoperative results.
Lipofilling can be performed under either local or general anaesthesia. Local anaesthesia is only used when small volumes of fat are required. The donor site is always infiltrated with a mixture of local anesthesia and adrenaline to reduce post-operative discomfort and bruising.
 |
 |
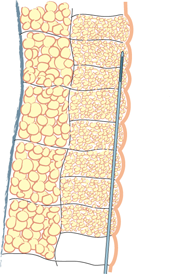 |
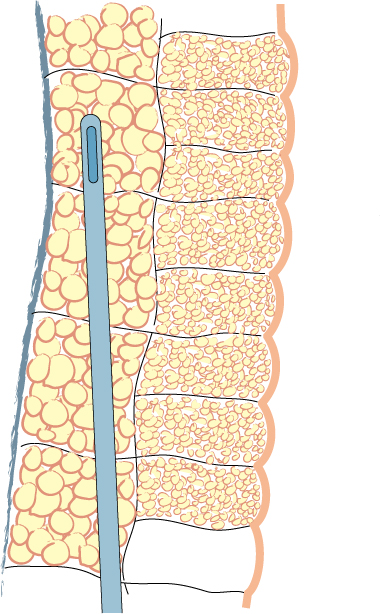
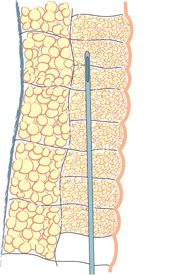
| Fig. 1a | Fig. 1b | Fig. 1c |
Fig. 1: Liposuction of the subcutaneous fat is performed using a 3mm. cannula in the deepest layer (a), a 2 to 3 mm. cannula in the intermediate layer (b) and a 2 mm. cannula in the most superficial layer (c).
Lipofilling takes between 45 minutes and 3 hours, depending on the volume of fat to be transferred. The fat is harvested through 5mm incisions placed within skin creases, such as the lower buttock fold or areas that are commonly hidden by underwear. Two to 3mm cannulas are used, but the more superficial the harvest, the thinner the cannula (fig. 1). The fat is aspirated at either high or low negative pressure, depending on the indication and the surgeon’s preference.

Fig. 2: The aspiration cannula connected to the “fat trap”. This collecting canister is connected by a tube to a negative pressure device or liposuction machine (seen in the background).
Fat is collected in a specially designed canister (fig. 2) and then transferred into smaller receptacles, typically 10 to 20 cc syringes, which are centrifuged for 2 to 3 minutes. This separates the components into oil, water and the cellular fraction, consisting mainly of fat and stem cells. The oil and water are then discarded and the cellular fraction is preserved. The cellular fraction is transferred into 1, 5 or 10 cc syringes depending on the volume to be injected and the recipient site (fig.3). The donor site incisions are then closed with absorbable sutures and small dressings applied.
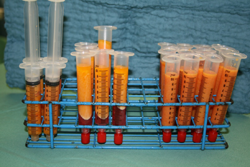
Fig. 3: The different filtration phases: (right) the aspirated fluid transferred from the collecting container into syringes; (middle) after centrifugation, separation of the aspirated fluid into a water layer at the bottom, cellular fraction in the middle, and the oil layer on top; (left) after the water and oil have been discarded, the cellular fraction is ready for injection.
The fat is injected through cannulas that measure only 1 to 2.5 mm in diameter (fig. 4). This leaves virtually no scarring at the recipient site. The subcutaneous layer is injected by making hundreds or thousands of passes through the same incision and depositing microscopic particles of fat on each occasion. This creates multiple small tunnels, in opposing directions, throughout the soft tissue layer.

Fig. 4: typical injection canula
The injected fat initially survives by receiving oxygen and nutrients from its surroundings but this source is gradually depleted. At the same time, new blood vessels are growing towards the fat grafts (neo-angiogenesis), which are sending out distress signals. If the fat particles are too large (more than 3mm) or grouped too closely together, the blood vessels will not be able to reach them in time. The central part of the fat graft then remains de-vascularized and will die. Any dead fat turns into oil and the body isolates this by creating a cyst. Cysts may be spontaneously resorbed but if they are too big, they have to be surgically removed.
Further details of the technique are available at: www.lipofilling.com
Pre-operatively
It is vitally important that you discuss your expectations. In many cases two or three attempts at lipofilling may be necessary to achieve the desired effect. Unfortunately, approximately 50% of the injected fat is reabsorbed after each procedure and every patient needs to be aware of this.
Different scientific studies report fat survival rates of between 30 and 75%. Fat loss is due to trauma during surgery, deposits that are too large, apoptosis (programmed cell death) or other destructive cellular mechanisms. This means that overcorrection may be necessary but, the volume of fat that can be injected on one occasion is limited by the thickness and laxity of the soft tissue at the recipient site.
In general, there are two significant volume decreases following surgery (fig. 5):
- The first is at approximately 3 weeks, when the post-operative fluid accumulation (oedema) settles.
- The second occurs 4 to 6 months later as dead fat cells are reabsorbed by the body.
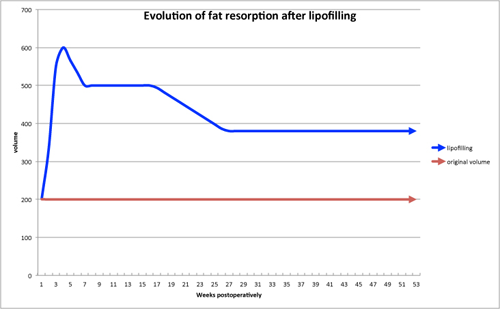
Fig. 5: A graph indicating the reabsorption pattern of structural fat grafts: the first decrease is due to oedema settling and the second decrease is due to reabsorption of the dead fat cells.
In this example: day O: 200cc original volume, 300 cc lipofilling; at 3 weeks: total volume consisting of 200cc original volume, 300cc lipofilling, 100cc edema; at 6 weeks: total volume consisting of 200cc original volume, 300cc lipofilling; at 6 months: total volume consisting of 200cc original volume, 180 cc of the grafted fat cells have survived.
The fat cells that survive add volume to the area that lasts a lifetime but hormonal and weight changes may be responsible for future gains or losses.
To improve the surgical outcome, patients are encouraged not to smoke. Smoking decreases fat graft survival and increases the risk of complications, particularly delayed wound healing.
Post-operatively
Many patients experience areas of numbness post-operatively. This is related to swelling, mild trauma to the sensory nerves and the fact that local anaesthetic was administered. In addition, it is very common to develop bruising in the areas where the fat has been harvested and injected.
You will be asked to wear special compression garments after your surgery. These reduce swelling and bruising at the donor sites and the pressure also facilitates skin retraction and re-attachment of the underlying soft tissues. The compression garments are worn continuously, day and night, for 4 to 6 weeks. They may be removed briefly to wash or shower.
Do not place any ice or constrictive clothing, e.g. a bra, over the recipient area for 3 weeks. This enables the new budding blood vessels to penetrate the fat grafts. Smoking also stops the formation of these blood vessels and is completely forbidden.
You may need to take regular analgesia for a few days as lipofilling can cause some discomfort. In addition, refrain from driving until you feel comfortable and able to perform an emergency stop, if necessary. You should not do any housework or heavy lifting for at least 7 days. Most patients return to work 10-14 days following their surgery but sport should be avoided for at least 4 weeks.
Post-operative complications
Common sequelae:
- Discomfort
- Transient numbness
- Bruising
- Swelling
General complications:
- Haematoma (<1%) which may require a return to theatre
- Wound infection (<1%)
- Seroma (<5%)
- Hypertrophic scars
Complications specific to this procedure:
- Subcutaneous cysts, nodules or scarring
- Fat reabsorption requiring additional surgery
Advantages and disadvantages
Advantages:
- Improvement at both the recipient site and the area from where fat is harvested.
- Surviving fat is permanent.
- A completely natural material.
- Day surgery, minimal discomfort and a short recovery.
- Minimally invasive, with a low risk of complications.
- Small scars at the donor site and no additional scars at the recipient site.
- Improves the quality of the overlying skin. This can be particularly important following radiation damage or in facial rejuvenation procedures.
Disadvantages
- Repeated procedures may be necessary.
- Lipofilling only adds volume, not additional skin. If this is required, for example after breast cancer surgery, local or distant flaps cannot be avoided.
- Lipofilling is not possible if you are very thin.
- Hormonal or weight changes may be responsible for future gains or losses.
- Lipofilling may not be covered by your insurance policy. Please check.
References
Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg 2007;119(3):775e85.
Spear SL, Newman MK. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg 2007;119(3):786e7.
Khouri R, Del Vecchio D. Breast reconstruction and augmentation using pre-expansion and autologous fat transplantation. Clin Plast Surg. 2009;36(2):269-80.
Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg. 2009;33(5):706-15.
Petit JY, Lohsiriwat V, Clough KB, Sarfati I, Ihrai T, Rietjens M, Veronesi P, Rossetto F, Scevola A, Delay E. The oncologic outcome and immediate surgical complications of lipofilling in breast cancer patients: a multicenter study--Milan-Paris-Lyon experience of 646 lipofilling procedures. Plast Reconstr Surg. 2011;128(6):1317.
Rigotti G, Marchi A, Stringhini P, Baroni G, Galiè M, Molino AM, Mercanti A, Micciolo R, Sbarbati A. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthetic Plast Surg. 2010;34(4):475-80.

 Céline Zorn, sage-femme, coach de vie et praticienne en hypnose allie ses différents domaines d’expertise et son expérience ...
Céline Zorn, sage-femme, coach de vie et praticienne en hypnose allie ses différents domaines d’expertise et son expérience ... Voilà trois semaines que nous sommes rentrées, c'était formidable et nous avons profité chaque instant de cette magnifique aventure.
Voilà trois semaines que nous sommes rentrées, c'était formidable et nous avons profité chaque instant de cette magnifique aventure. Venus médical s’engage dans le processus de reconstruction mammaire. L’esthétique est terriblement importante ...
Venus médical s’engage dans le processus de reconstruction mammaire. L’esthétique est terriblement importante ... Soutenez notre association avec le verre BABC de l'amitié
Soutenez notre association avec le verre BABC de l'amitié